Introduction to Patient Monitoring
Chronic Care Management (CCM), Telehealth, and Remote Patient Monitoring (RPM) are distinct modalities of digital health that can use telecommunications to allow providers to monitor their patients and deliver care outside the office.
CCM
CCM is the coordination of medical care provided outside the regular office visit for patients with 2 or more chronic conditions expected to last at least 12 months or until the death of the patient and that place the patient at significant risk of death, acute exacerbation or decompensation, or functional decline.1
TELEHEALTH
RPM
RPM is the use of digital technologies to receive physiologic data electronically from patients in one location and send it to healthcare providers (HCPs) in a different location for assessment and recommendations.6
CCM, Telehealth, and RPM services have similar components, but there are some key differences to note between them.
- Non-complex and complex billing codes
- More than 2 chronic conditions
- Established or non-established patients can use the service
- 20-60 minute billing periods

- Primarily Medicare beneficiaries
- Services include telehealth visits, virtual check-ins, E-visits

- Use of a medical device that can transmit data from patient to provider
- Acute or chronic conditions
- Established patient–physician relationship required
- 20-30 minute billing periods

CPT Codes for Reimbursement
Data from the website is shared for informational purposes only. Please note that the codes below and all information on reimbursement is subject to change based on the discretion of the Centers for Medicare and Medicaid Services (CMS). Specific guidance on the submission of claims provided by the CMS or other payers supersedes the codes listed below. Providers are responsible for the accuracy of any claims, invoices, or related documentation submitted to payers.
CPT codesCCM services are categorized as7:
- Non-complex CCM
- Complex CCM
It is important to note that all CPT codes for CCM services include1:
- Multiple (2 or more) chronic conditions expected to last at least 12 months, or until the death of the patient
- Chronic conditions that place the patient at significant risk of death, acute exacerbation/decompensation, or functional decline
- Establishing, implementing, revising, or monitoring a comprehensive care plan
Non-complex CCM
99490
Chronic care management services, at least 20 minutes of clinical staff time directed by a physician or other qualified healthcare professional (QHCP), per calendar month
Additional Requirements:
- Requires a minimum of 15 minutes of work by the physician or QHCP, per month
- Comprehensive care plan established, implemented, revised, or monitored
99491
Chronic care management services, provided by a physician or other QHCP, at least 30 minutes of physician or other QHCP time, per calendar month
Additional Requirements:
- Comprehensive care plan established, implemented, revised, or monitored
G2058
Chronic care management services, each additional 20 minutes of clinical staff time directed by a physician or QHCP, per calendar month (list separately in addition to code for primary procedure)
Additional Requirements:
- Do not report code G2058 for care management services of less than 20 minutes in addition to the first 20 minutes of CCM services during a calendar month
- CPT code G2058 must be reported in conjunction with code 99490
- Do not report codes 99490 or G2058 in the same calendar month as codes 99487, 99489, 99491
Complex CCM
CPT CODE
DESCRIPTION AND BILLING FREQUENCY1
99487
Chronic care management services, involving establishment or substantial revision of a comprehensive care plan, moderate or high complexity medical decision making, and 60 minutes of clinical staff time directed by a physician or other QHCP, per calendar month
99489
Chronic care management services, each additional 30 minutes of clinical staff time directed by a physician or other QHCP, per calendar month (list separately in addition to code for primary procedure)
Additional Requirements:
- Complex CCM services of less than 60 minutes in duration, in a calendar month, are not reported separately
- CPT code 99489 must be reported in conjunction with code 99487
- Do not report code 99489 for services of less than 30 minutes in addition to the first 60 minutes of complex CCM services in the same calendar month
Medicare Telehealth Visit Codes
The table below displays a partial list of codes that are used to bill for Medicare telehealth visits. For the complete list of codes, please visit https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/
MLNProducts/Downloads/
TelehealthSrvcsfctsht.pdf
CPT CODE
DESCRIPTION AND BILLING FREQUENCY13
G0425-G0427
Telehealth consultations, emergency department or initial inpatient visits
G0406-G0408
Follow-up inpatient telehealth consultations furnished to beneficiaries in hospitals or skilled nursing facilities (SNFs)
99201-99215
Office or other outpatient visits
99231-99233
Subsequent hospital care services, with the limitation of 1 telehealth visit every 3 days
99307-99310
Subsequent nursing facility care services, with the limitation of 1 telehealth visit every 30 days
Virtual Check-in Codes
Codes G2012 and G2010 both require the patient’s consent in advance and are covered for established patients.9 Providers may educate patients on the availability of the service prior to the patient agreement.10
CPT CODE
DESCRIPTION AND BILLING FREQUENCY9
G2012
Brief communication technology-based service by a physician or other QHCP who can report evaluation and management (E/M) services, not originating from a related E/M service provided within the previous 7 days nor leading to an E/M service or procedure within the next 24 hours or soonest available appointment; 5-10 minutes of medical discussion
No frequency limitations
Additional Requirements:
- Technology used can be real-time audio-only telephone interactions and synchronous, 2-way audio interactions that are enhanced with the video or other kinds of data transmission
- Telephone calls that involve only clinical staff cannot be billed and reimbursed using this code
G2010
Remote evaluation of recorded video and/or images submitted by a patient, including interpretation with follow-up with the patient within 24 business hours, not originating from a related E/M service provided within the previous 7 days nor leading to an E/M service or procedure within the next 24 hours or soonest available appointment
Additional Requirements:
- Services can include using a patient-generated still or video image to determine if an in-office visit is required
- Provider may follow-up with the patient via phone call, audio or visual communication, secure text messaging, email or patient portal and MUST be HIPAA-compliant
E-visit Codes
All codes for E-visits are covered for established patients.10 Individual services need to be initiated by the patient, but providers may educate the patients on the availability of the service prior to the patient agreement.10
CPT CODE
DESCRIPTION AND BILLING FREQUENCY10
99421
Online digital E/M service, for up to 7 days, cumulative during the 7 days; 5-10 minutes
99422
Online digital E/M service, for up to 7 days, cumulative during the 7 days; 11-20 minutes
99423
Online digital E/M service, for up to 7 days, cumulative during the 7 days; 21 or more minutes
G2061
QHCP online assessment and management, for up to 7 days, cumulative time during the 7 days, 5-10 minutes
G2062
QHCP online assessment and management, for up to 7 days, cumulative time during the 7 days, 11-20 minutes
G2063
QHCP online assessment and management, for up to 7 days, cumulative time during the 7 days, 21 or more minutes
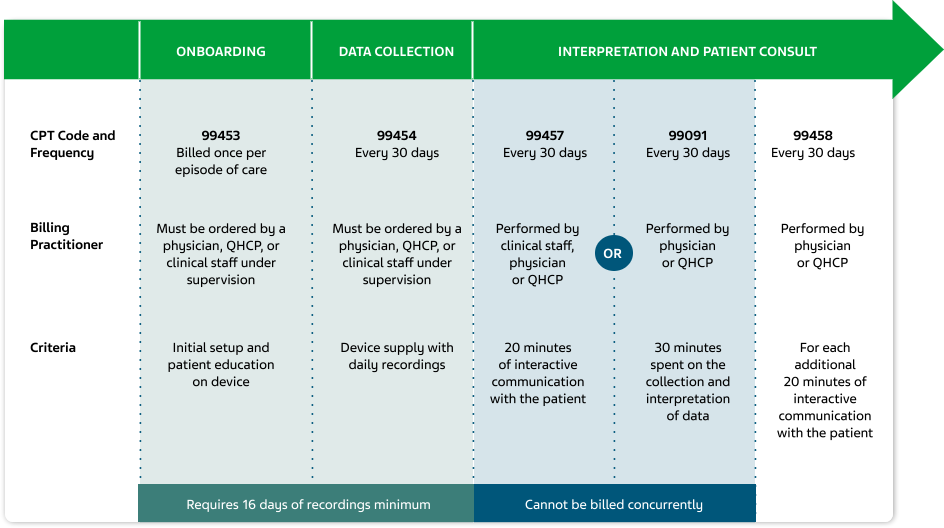
99091
Collection and interpretation of physiologic data (eg, ECG, blood pressure, glucose monitoring) digitally stored and/or transmitted by the patient and/or caregiver to the physician or other QHCP, qualified by education, training, licensure/regulation (when applicable)
Requiring a minimum of 30 minutes of time per patient per month, every 30 days
Additional Requirements:
- An in-patient visit prior to service
- Includes evaluation/management (E/M) services, preventative physical exam, translational care management
- Does not include virtual face-to-face visits using other variations of telehealth
- Billing is limited to once in a 30-day period
CMS will reimburse for professional time dedicated to monitoring services and does not require interactive communication to bill. Codes 99457 and 99091 cannot be billed concurrently.
99453
Remote monitoring of physiologic parameter(s) (eg, weight, blood pressure, pulse oximetry, respiratory flow rate), initial set-up and patient education on use of equipment
CPT code 99453 offers reimbursement for the work associated with onboarding a new patient onto a RPM service, setting up the equipment and educating the patient on using the equipment.
99454
Device(s) supply with daily recording(s) or programmed alert(s) transmission, each 30 days
CPT code 99454 offers reimbursement for providing the patient with a RPM device for a 30-day period. Note that code 99454 can be billed each 30 days.
99457
Remote physiologic monitoring treatment management services, 20 minutes or more of clinical staff/physician/other QHCP time in a calendar month requiring interactive communication with the patient/caregiver during the month
First 20 minutes per patient per month
CMS will reimburse for clinical staff time that contributes toward monitoring and interactive communication.
99458
(New in 2020)
Remote physiologic monitoring treatment management services, clinical staff/physician/other QHCP time in a calendar month requiring interactive communication with the patient caregiver during the month
First 20 minutes per patient per month
Additional Requirements
(99453-54, 57-58):
- Billing is limited to once in a 30-day period
- Codes 99457 and 99091 cannot be billed together for same billing period and patient
*Use of all codes require providers to obtain patient consent to use the service in advance, and have it documented in the patient’s chart. **This guide will be updated over time to reflect changes in additional guidance that CMS is expected to provide for these highlighted services. All questions concerning CMS requirements should be addressed to the relevant Medicare contractor in your region.
Billing Process for RPM9,14,15

Additionally, providers should take the following points in to consideration to bill and receive reimbursement for RPM8:
An established patient–physician relationship will be required for RPM services to be provided
Patient consent can be obtained at the time that RPM services are provided
Device supplied to the patient under
CPT code 99454 must be a medical
device as defined by Section 201(h) of
the Federal Food, Drug, and Cosmetic Act
- Data must be electronically collected and transmitted rather than
self-reported
RPM services may be provided to patients with acute or chronic conditions
Impact of COVID-19
Medicare
Reimbursement
for Telehealth
Beginning
March 6, 2020,
Medicare will pay for office,
hospital, and other visits
provided via telehealth in
patient’s residences and
across the country10
Same In-Office
Pay Rate
for Physicians
Physicians will be
paid the same rate for
telehealth services as done
for in-office visits, for all
diagnoses (not just specific
to COVID-19)16
Reducing
Patient Travel
Medicare can now pay for
telehealth services provided to
patients outside of designated
rural areas without having them
leave their homes to visit
a healthcare facility10
Billing for Less
Than 16 Days of
RPM Services
Allow billing for
monitoring less than
16 days in a 30-day RPM billing
period, for the treatment of
suspected COVID-19 infections;
as long as other code
requirements are met17
Reducing or Waiving
Cost-Sharing for Patients
The HHS Office of Inspector
General (OIG) is allowing providers
to reduce or waive cost-sharing for
telehealth services paid for by
federal healthcare programs10
FAQs 
Chronic Care Management (CCM)
Is a new patient consent required each calendar month or annually to bill for CCM services?
New consent is only required if the patient changes billing practitioners, as stated in the 2014 PFS final rule with comment period (78 FD 74424). In this case, the new billing practitioner must obtain and document the patient’s consent before providing CCM services.18
Can all CCM CPT codes be billed together for the same patient by the same practitioner for each billing period?
The CPT code descriptors state that only one type of CCM service (non-complex CCM or complex CCM) can be provided per billing period. CPT code 99491 cannot be reported for the same calendar month as CPT codes 99487, 99489 or 99490.18
CPT codes 99487 and 99489 for complex CCM cannot be reported within the same calendar month as any other CCM service code. However, these 2 CPT codes may be reported together during the same calendar month, as long as the time requirement for each code is met.18
Can practitioners bill and get reimbursed for face-to-face activities?
CCM services include the coordination of medical services provided outside the regular office visit (via telecommunications). This can comprise reviewing medical records and test results, patient education, motivational counseling, and exchange of health information with other practitioners and providers. Prior to separate reimbursement codes for CCM, these types of services were typically billed for in face-to-face office visits as “non-face-to-face” activities.18
If the billing practitioner believes that a particular patient receiving CCM services would benefit from or engage more via a face-to-face visit, they may count that time and effort as billable time. However, that time and effort cannot count towards any other code if they are counted towards CCM.18
Telehealth
What if a patient does not have access to a smartphone or other technology that supports 2-way audio and video telecommunications? What if the patient does not want to use video?
Beginning on March 1, 2020, providers can bill for certain Medicare telehealth services via audio-only calls. This includes telephone E/M services, and specific behavioral healthcare and educational services for both new and established patients.16
Is patient consent required for virtual check-ins, E-visits, audio-video telehealth visits, and/or telephone-only E/M telehealth visits?
Patient consent for virtual check-ins and E-visits is required at least once annually. During the PHE, however, consent may be obtained once at the same time that the service is provided. The patient’s consent is not required to be noted in the medical record for telehealth services provided using interactive audio-video technology and audio-only phone visits.16
How are telehealth services different from virtual check-ins and E-visits?
Medicare telehealth services are services that would normally occur in person but are instead conducted via real-time, 2-way telecommunications. These services are billed and reimbursed at the full in-person rate.16
Virtual check-ins, E-visits, remote evaluation, and telephone visits are services that would not normally occur in person. Therefore, these services are not billed and reimbursed as though the service occurred in person.16
Remote Patient Monitoring (RPM)
Can RPM services be provided to new patients as well as established patients?
Effective March 1st, 2020 and for the duration of the PHE, RPM services can be provided to both new and established patients. CMS is not requiring patients to be established in an initial visit in order to receive RPM services. Please note that this is an exception for the duration of the PHE only.16
RPM CPT Codes 99453 and 99454 require a minimum of 16 days of monitoring per 30-day billing period in order to be reimbursed. Does this apply to patients diagnosed with COVID-19 who may not necessarily require 16 days of continuous monitoring?
The CMS has established a policy for the duration of the PHE that allows monitoring for fewer than 16 days of the 30-day billing period, but no less than 2 days (as long as the other requirements for billing the code are met). However, the patient must have a confirmed or suspected case of COVID-19 in order for practitioners to bill and get reimbursed for less than 16 days of monitoring under these CPT codes.16
RPM CPT codes 99453, 99454, and 99457 state that the device used to transmit physiologic data must be a medical device as defined by the FDA. Would any device that fulfills this criterion meet the FDA requirement?
The FDA will consider a product to be a medical device that is subject to regulation if it meets the definition of a medical device per Section 201(h) of the Food, Drug, and Cosmetic Act. It is important to clarify that the CPT code descriptors do not directly indicate that the device must be an FDA-approved device. For more information on what this means, visit the FDA’s webpage on “How To Determine if Your Product is a Medical Device” at https://www.fda.gov/medical-devices/classify-your-medical-device/how-determine-if-your-product-medical-device.16
References: 1. Chronic Care Management Services. Centers for Medicare and Medicaid
Services. Accessed December 6, 2020. https://www.cms.gov/outreach-and-education/
medicare-learning-
network-mln/mlnproducts/downloads/
chroniccaremanagement.pdf. 2. General Provider Telehealth and Telemedicine Tool
Kit. Centers for Medicare and Medicaid Services. Accessed December 6, 2020. https://
www.cms.gov/files/document/general-telemedicine-toolkit.pdf. 3. Telehealth. Medicare.gov. Accessed December 6, 2020. https://www.medicare.gov/coverage/
telehealth. 4. Virtual
check-ins. Medicare.gov. Accessed December 6, 2020. https://
www.medicare.gov/coverage/virtual-check-ins. 5. E-visits. Medicare.gov. Accessed December 6, 2020. https://www.medicare.gov/
coverage/e-visits. 6. Remote Patient Monitoring (RPM). Center for Connected Health Policy. Accessed December 6, 2020. https://www.cchpca.org/about/about-telehealth/remote-patient-
monitoring-rpm.
7. Connected Care Toolkit Chronic Care Management Resources for Healthcare
Professionals and Communities. Centers for Medicare and Medicaid Services. Accessed
December 6,
2020. https://www.cms.gov/About-CMS/Agency-Information/OMH/
Downloads/connected-hcptoolkit.pdf. 8. Proposed Policy, Payment, and Quality
Provisions Changes to the Medicare Physician
Fee Schedule for Calendar Year 2021.
Centers for Medicare and Medicaid Services. August 3, 2020. Accessed December 6,
2020. https://www.cms.gov/newsroom/fact-sheets/proposed-policy
-payment-and-quality-provisions-changes-medicare-physician-fee-schedule-calendar-year-4. 9. Navigating Digital Medicine Coding and Payment. American Medical Association.
Accessed
December 6, 2020. https://www.ama-assn.org/system/files/2018-12/
playbook-resources-step-5-coding-payment-REV1.pdf. 10. Medicare Telemedicine
Health Care Provider Fact Sheet. Centers for Medicare and Medicaid Services. March
17, 2020. Accessed December 6, 2020. https://www.cms.gov/newsroom/fact-sheets/
medicare-telemedicine-health-care-provider-fact-sheet.
11. Using
Telehealth to Expand Access to Essential Health Services During the
COVID-19 Pandemic. Centers for Disease Control and Prevention. Updated June 10,
2020. Accessed December 6, 2020. https://
www.cdc.gov/coronavirus/2019-ncov/hcp/
telehealth.html. 12. Summary of Policies in the Calendar Year (CY) 2020 Medicare Physician Fee Schedule (MPFS) Final Rule, Telehealth Originating Site
Facility Fee Payment Amount and Telehealth Services List, CT Modifier Reduction List, and Preventive Services List. Centers for Medicare and Medicaid Services. Accessed December 6, 2020. https://
www.cms.gov/files/document/mm11560. 13. Telehealth Services. Centers for Medicare and Medicaid Services. Accessed December 6, 2020. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/
MLNProducts/Downloads/TelehealthSrvcsfctsht.pdf. 14. CMS-1693-F. Centers for Medicare and Medicaid Services. Accessed December 6, 2020. https://www.cms.gov/
Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/PFS-Federal-Regulation-Notices-Items/CMS-1693-F. 15. CMS-1715-F. Centers for Medicare and Medicaid Services. Accessed
December 6, 2020. https://www.cms.gov/Medicare/
Medicare-Fee-for-Service-Payment/PhysicianFeeSched/PFS-Federal-Regulation-Notices-Items/CMS-1715-F. 16. COVID-19 Frequently Asked Questions (FAQs) on Medicare Fee-for-Service (FFS) Billing. Centers for Medicare and Medicaid Services. Updated December 3, 2020. Accessed December 6, 2020. https://www.cms.gov/files/
document/03092020-covid-19-faqs-508.pdf. 17. Physicians and Other Clinicians: CMS Flexibilities to Fight COVID-19. Centers for Medicare and Medicaid Services. Accessed December 6, 2020. https://www.cms.gov/files/document/covid-19-physicians-and-practitioners.pdf. 18. Frequently Asked Questions about Physician Billing for Chronic Care Management Services. Centers for Medicare
and Medicaid Services. Updated November 4, 2020. Accessed December 6, 2020. https://www.cms.gov/Medicare/
Medicare-Fee-for-Service-Payment/PhysicianFeeSched/Downloads/
Payment_for_CCM_Services_FAQ.pdf.